Aug 17, · Writing in a SOAP note format—Subjective, Objective, Assessment, Plan—allows healthcare practitioners to conduct clear and concise documentation of patient information. This method of documentation helps the involved practitioner get a better overview and understanding of the patient’s concerns and blogger.comted Reading Time: 5 mins Points to note: This is the most important part of a SOAP notes as it will help you in the objective part when trying to get to the Make sure you completely avoid any question that will result in a YES or NO answer. Do not pre-judge on the patient, for example, thinking that the patient is Estimated Reading Time: 10 mins Because SOAP notes are employed by a broad range of fields with different patient/client care objectives, their ideal format can differ substantially between fields, workplaces, and even within departments. However, all SOAP notes should include Subjective, Objective, Assessment, and Plan sections, hence the acronym SOAP. A SOAP note should convey information from a session that the
How to Write a SOAP Note: Detailed Guide and Samples
This page is brought to you by the OWL at Purdue University. When printing this page, you must include the entire legal notice. All rights reserved. This material may not be published, reproduced, writing soap notes, broadcast, rewritten, or redistributed without permission.
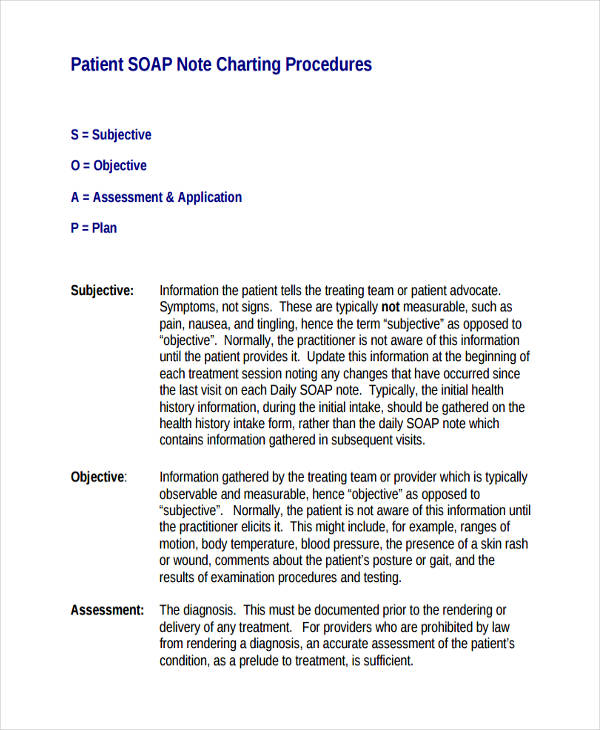
Use of this site constitutes acceptance of our terms and conditions of fair use. This resource provides information on SOAP Notes, which are a clinical documentation format used in a range of healthcare fields. The resource discusses the audience and purpose of SOAP notes, suggested content for each section, and examples of appropriate and inappropriate language. A SOAP note is a form of written documentation many healthcare professions use to record a patient or client interaction.
However, all SOAP notes should include SubjectiveObjectiveAssessmentand Plan sections, hence the acronym SOAP. A SOAP note should convey information from a session that the writer feels is relevant for other healthcare professionals to provide appropriate treatment.
A good SOAP note should result in improved quality of patient care by helping healthcare professionals better document and therefore recall and apply details about a specific case.
SOAP notes can be written in full sentence paragraph form or as an organized list of sentences fragments.
Note writing soap notes difference in style and format in the following two examples. The first come from within a hospital context. The second is an example from a mental health counseling setting.
S Reports counseling is not helping him get his family back, writing soap notes. Reports history of domestic violence. Recent history: States he met and verbally fought with his wife yesterday regarding the privileges of oldest child. Personal history: childhood physical and mental abuse resulting in foster care placement, ages O Generally agitated throughout the session, writing soap notes. A Physical Abuse of Adult [V Clinical impressions: rule out Intermittent Explosive Disorder given bouts of writing soap notes rage with non-specific emotional trigger.
Cameron, Ph. These examples are not the only two ways to write a SOAP note. Rather, they showcase differences in approaches for SOAP note styles. As mentioned above, different fields and even different clinics will have varied preferences and practices for writing these clinical documents. Conversely, also keep in mind that efficiency and time management are important in the healthcare professions. To save both the writer and reader time, avoid overly wordy phrasing and unnecessary detail.
It is perfectly acceptable and often encouraged in many settings to writing soap notes abbreviations when writing SOAP notes. In some writing soap notes, especially those that use electronic healthcare records, the writer will be constrained to a predetermined number of characters that can be entered. Learning to write case notes using the SOAP format. Heifferon, Barbara A. Writing in the health professions. Find Info For Find Info For Academics Admissions Current Students Athletics About Careers Prospective Students Research and Partnerships Quick Links Apply News President Shop Visit Give Emergency.
Purdue Online Writing Lab College of Writing soap notes Arts. Writing Lab Purdue OWL Research Contact Site Map. Subject-Specific Writing Healthcare Writing SOAP Notes. Welcome to the Purdue OWL This page is brought to you by the OWL at Purdue University.
SOAP Notes Summary: This resource provides information on SOAP Notes, which are a clinical documentation format used in a range of healthcare fields.
How to Write SOAP Format for Mental Health Counselors
, time: 6:48How to Write a SOAP Note: Writing Guide - A Research Guide for Students
Points to note: This is the most important part of a SOAP notes as it will help you in the objective part when trying to get to the Make sure you completely avoid any question that will result in a YES or NO answer. Do not pre-judge on the patient, for example, thinking that the patient is Estimated Reading Time: 10 mins Because SOAP notes are employed by a broad range of fields with different patient/client care objectives, their ideal format can differ substantially between fields, workplaces, and even within departments. However, all SOAP notes should include Subjective, Objective, Assessment, and Plan sections, hence the acronym SOAP. A SOAP note should convey information from a session that the Aug 03, · How does a SOAP note work? Record checklist details. In this SOAP Note Template, you will be presented with the following form fields which you are Subjective. Document what the patient tells you. The subjective section refers to what the patient tells you. Use the Estimated Reading Time: 8 mins
No comments:
Post a Comment